 Pope Clement VI hired several plague doctors during the Black Death – by 1848, only one of Venice's original 18 doctors remained. The nose mask 'protected' them from contagion. Pope Clement VI hired several plague doctors during the Black Death – by 1848, only one of Venice's original 18 doctors remained. The nose mask 'protected' them from contagion. For most of human history contagious disease has been something you would go out of your way to avoid, or at least try to avoid, the Black Death being a case in point. The bubonic plague which fueled the Black Death, killed off close to 100 million people across greater Europe, about half of all Europeans at the time. Nothing could stop it, certainly not the traveling plague doctors who roamed Europe at the time. Peaking around 1350 AD, the pandemic was caused by miniscule bacteria carried around by fleas. Somewhat ironically, seen from today’s perspective, climate change was indirectly responsible... the fleas carrying the disease having been transported by rodents escaping Central Asia, where it had become too dry to support their lives. Today, the impact of such an infectious disease, were it to occur, would be nothing like on the scale of what it was back then, or more specifically, it would kill a lot less people. We’ve got very good at tackling bacterial and virus borne diseases even while acknowledging that some of our medicines are less effective than they once were. In a nutshell, the way society thinks about such communicable diseases in general has changed – we have mastered them. We know that if we get ill, there’s a box of pills or a syringe full of antibiotics waiting to save us. We think we have the upper hand, but truth be told, we don’t, because we are blind to the current, albeit quite different type of plague which is increasingly affecting individuals and society as a whole. The current plague is being lived every day by people all around us, bringing with it devastating outcomes; we just don’t notice it, or at least, we don’t talk about it in anything like the same way as we would say, with bubonic plague. The reasons are twofold. First, the Black Death was communicable, making it both terrifying and all too often heartbreaking for families and friends. Trying to avoid it, meant staying away from the disease carriers, those being fleas, rodents or the sick people in your vicinity - if you could; and yet, most could not. The other reason was that if you got sick, you didn’t have long to live; almost no-one recovered. You got ill, suffered badly and died in a horrible way, all within a few weeks. Today's plague has no name The way diseases of civilization (NCDs) are treated today is akin to slowing down a train crash video. The awful result is inevitable, but at least you can delay it. The way diseases of civilization (NCDs) are treated today is akin to slowing down a train crash video. The awful result is inevitable, but at least you can delay it. Today’s plague does not present as an illness followed by a quick death. Today’s plague does not even have a name (as yet) - at least not one upon which experts can agree. Today’s plague is more akin to watching a slow-motion train crash where the tragic result is inevitable but you have no influence on the process or the conclusion. You can only delay the result by playing the video even more slowly, or in medical terms, upping the doses of life-prolonging medicine. But today's plague should be revealed, it deserves a name. The name of our twenty-first century plague is hyperinsulinemia – in essence, an excess of insulin circulating around your body. An increasing number of doctors and researchers believe this to be the underlying cause of a large, mixed bag of chronic diseases ranging from type-2 diabetes to many forms of cancer and of course heart disease. It is associated with ailments as far apart as tinnitus and polycystic ovary syndrome and is increasingly associated with the hardening of arteries. Hyperinsulinemia does not necessarily make you obese but if you are, it is most likely the root cause of your excess weight – obesity being simply a marker for your future ailments. 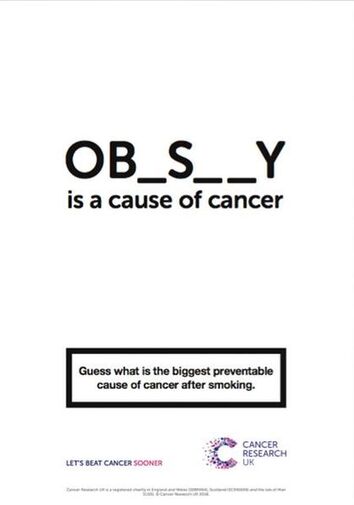 True, there is a strong association, but is it a root cause? True, there is a strong association, but is it a root cause? Much research focuses on the topic of obesity as do the headline writers. It’s easier to put together a story with strong visual impact, and Cancer Research UK’s posters recently warned that obesity has overtaken smoking as the leading cause of major cancers. Research from Harvard in 2017 led to the prediction that more than half (57%) all American children will be obese by the age of 35. But far from being portrayed as a potential disaster, a veritable plague of obesity, many argue that this just represents a shift to a new normal. Others link this rise in average body weight to fat shaming and increasing psychological abuse. In this context, you will also find discussions about healthier snacks and (misguided) recommendations about adding more fibre, fruit and vegetables to your diet, but seldom any root cause analysis. Even Cancer Research UK, when declaring that ‘obesity is a cause of cancer’ only provides us with part of the story. Hyperinsulinemia presents as the most basic, deepest, root cause. Over 10 years ago, a team led by Michael Shanik noted that, “Hyperinsulinemia, insulin resistance, and impairment of glucose-stimulated insulin release are intertwined biologically.” A single process (hyperinsulinemia) could generate all three simultaneously they suggested (Shanik, 2008). More recently, researchers have put forward a convincing case for unifying most of today’s chronic disease under that one term (Crofts, 2015), but in spite of growing awareness, there is still no mainstream acceptance. Type-2 diabetes provides us with the most obvious direct association and it is distressing to note that across the US, over 200 people per day have their legs amputated as a result of related complications. Up to 50% of them die within the following year although no-one talks about that much. Media headlines are likely to feature quicker, more spectacular deaths such as crashes, suicides and military interventions. We don’t really notice the steady stream of ‘non-communicable’ death around us, and diabetes-related deaths are just some of the many whose root cause lies in hyperinsulinemia. A new outbreak of bubonic plague on the other hand? Well… even if it were to only kill a few people, that would hit the headlines straight away, as you can well imagine. The fact of the matter is, we generally treat the symptoms of hyperinsulinemia related illnesses, but seldom the root cause. Most doctors and diabetes organizations do not know or even accept that it is the root cause. They prescribe medicines to slow down the effects of chronic disease, even when they bring their own unpleasant side effects. Ironically, this sometimes involves fanning the fire of disease by adding additional insulin. But does this high level of insulin running through the veins, arteries and organs of so many of us really constitute a plague… a word used generally for life-threatening infectious diseases? Does this make it a 'plague'?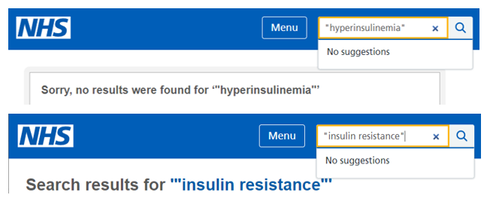 The NHS advice site doesn't acknowledge these words/phrases The NHS advice site doesn't acknowledge these words/phrases I argue that it does. Having an excess of insulin may not be infectious in the classically defined medical sense, but as a symptom of our modern civilization, it is strongly associated with our westernized ways of living. It only becomes rampant with the introduction of western eating habits and ultra-processed foods, as illustrated by the now common incidence of obesity and diabetes among previously healthy Pacific Islanders and the Inuit tribes of Canada. This plague is not transmitted by the touch or breath of another human, nor the bite of a single flea, yet it is transmitted by families and societies who have chosen to (or been encouraged, or forced to) move away from previously healthy foods associated with traditional dietary patterns. In the twenty-first century, we may have succeeded in removing the scourge of malnutrition – food shortage – from most of the world, but we have often replaced it with ‘mal-nutrition’ – food that fills you up but does not nourish you… leading all too easily to hyperinsulinemia. Does hyperinsulinemia even affect enough people to be called a plague or a pandemic? Do we even know how many people around the world suffer from it? Well, no one knows for sure. Britain’s NHS does not even acknowledge the term and although the Mayo Clinic suggests that hyperinsulinemia is most often caused by ‘insulin resistance’, that's another term which is not acknowledged by the NHS. We do however have the ‘metabolic syndrome’ which groups together diabetes, high blood pressure and obesity, all closely associated with hyperinsulinemia, so at least here, we have a starting point for establishing the number of sufferers. The International Diabetes Federation estimates that around 20-25% of the world’s adult population have the metabolic syndrome and states that they are twice as likely to die from and three times as likely to have a heart attack or stroke compared with people without the syndrome. The figures are higher for United States citizens, where the estimate is 30% - that’s about 100 million people alone in the US, although the Centre for Disease Prevention (CDC) estimates the figure to be even higher, putting it at over one third, and that was back in 2012. So, globally, it is likely to include more than one and a half billion of us. 1 1/2 billion! That extraordinary number is the real reason we should be talking about this, especially since those with the metabolic syndrome represent just a subset of all those suffering from hyperinsulinemia, the real root cause. Who benefits from root cause analysis?The big question remains; why do we still not recognise hyperinsulinemia as a global pandemic, a 21st century plague? And this is admittedly where my cynicism takes over. First, there are just too many highly trained specialists around who don’t always link up the dots between high insulin levels and say, cancer - not that it is necessarily in their interest to do so. I mean why open Pandora’s box, or in financial terms, why bite the hand that feeds you? Doctors and surgeons are trained to treat those of us in society who are sick, and they work really hard at it. But whose job is it to stop people getting sick in the first place? There is much more money in treatment than there is in prevention. As always, follow the money and the many vested interests. To be realistic, when it comes to prevention, while the epidemic remains unnamed and unrecognised, nothing much is likely to happen. If you don't even recognise the root cause 'problem', you are unlikely to come up with a solution. Although many acknowledge that the treatment of non-communicable disease will be the biggest medical and societal task of the 21st century, too few acknowledge (yet) that hyperinsulinemia is the principal underlying cause. Most of those in the front line occupy themselves with individual diseases and treatments; they simply cannot see the forest for the trees. And; there are still too many organizations and committees who’ve been blaming micro and macro factors such as sugar, saturated fat, salt, an excess of calories and too little exercise for our woes. Sugar is most certainly involved but… to adopt a more positive glass half-full attitude, wouldn’t genuine root cause analysis provide an opportunity to bring the scientific, dietetic and public health communities together? Controlling the plague by improving communication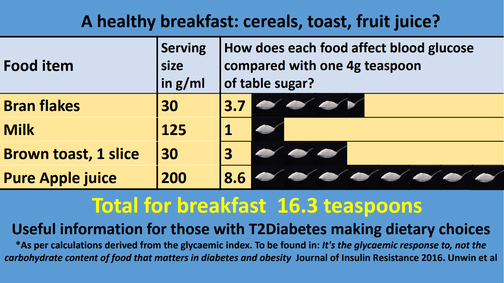 Courtesy of Dr Unwin and PHCUK – a brilliant portrayal of keeping communication simple Courtesy of Dr Unwin and PHCUK – a brilliant portrayal of keeping communication simple When treating individual metabolic diseases such as type-2 diabetes, we generally prescribe medicines which target the symptoms. Even taking a step back towards the root cause, we group together these connected diseases of civilization, using far too many different expressions, from diabesity to metabolic syndrome to insulin resistance and more. The proverbial man or woman in the street is rightfully confused. Yet we have learned that simple communication is the best communication. When you explain to a patient that their diabetes is caused by a growing intolerance to carbohydrates and give them some of Dr Unwin’s spoonful of sugar brochures, they get it; they know what to do. Tell them that they have metabolic syndrome or are becoming insulin resistant and they go… What? To simplify communication with the wider world, we should adopt a lesson from management text books – Keep It Simple Stupid (KISS). And in this context, there is one word to rule them all? Hyperinsulinemia, meaning ‘too much insulin’. Importantly, the pathway to treatment is provided in the word itself; and being self-explanatory makes it a more effective communications tool, in spite of its eight syllables. Interestingly, that might make it even more memorable (think: ‘do, re, mi, fa, sol, la, ti, do’, then say ‘hy, per, in, su, lin, e, mi, a'). Get it? By recognizing hyperinsulinemia as the real master-villain, the plague that it truly sums up, we do however open up interested parties to a potentially frightening thought: all these related diseases are curable or at least reversible through lifestyle interventions, most notably, lower-carbohydrate diets and most probably, a move away from ultra-processed food. And because the medical specialists and insurance organisations, the clinics, hospitals and drug companies make so much money from an old, communicative-disease model inherited from the world before this kind of chronic illness ruled the roost; what is their incentive for change? Well, there probably isn’t one, at least not in the short-term. But if all those involved could agree to focus their efforts on communicating this one word, 'hy per in su lin e mi a', at least we’d have a better starting position. Most importantly, it’s so much easier for the ‘layman’ to understand. Imagine a patient who’s just been told she is suffering from hyperinsulinemia, understanding immediately that ‘too much insulin’ is the core problem and coming up with questions like, “So, how can I reduce my insulin levels?” or “why on earth am I taking insulin then?”. Imagine her delight when the doctor answers that she can get results through challenging but easily achievable lifestyle interventions that begin in her own kitchen. Wouldn’t that be a good start? Thinking bigger and scarier = communicating better It seems obvious to treat the condition topically, yet the rash is truly a sign of 'the plague'. Again, we miss the root cause. The cream merely provides a temporary band-aid. It seems obvious to treat the condition topically, yet the rash is truly a sign of 'the plague'. Again, we miss the root cause. The cream merely provides a temporary band-aid. If you are still, as yet, unconvinced by these arguments for referring to hyperinsulinemia as a modern-day plague, here is one more reason. Perhaps I should say, a provocation. To promote change and make this topic newsworthy for journalists and other opinion leaders, we need to think bigger. Consider just one subset of our modern-day plague sufferers; those who exhibit skin ailments. Psoriasis and other insulin related skin conditions are still mostly treated with topical creams when in reality, they are linked to chronic inflammation which, in turn, is linked to metabolic factors, principally to excessive insulin circulating in the body (Gyldenlove, 2015). That’s why metformin and other hypoglycemic drugs are now being prescribed more frequently as methods of treatment. Admittedly, this represents a step along the root cause pathway but it still implies treatment of the symptoms rather than the true cause. Shock tactics? For bloggers and journalists, lifestyle adjustment stories that tackle the real problem would be stronger and more appealing if psoriasis were shown to be a sign of having the plague – a visual marker for hyperinsulinemia. Yes I did just write that. I am well aware that talking in such terms can be scary and potentially discriminatory but thankfully, we won’t need plague doctors to provide solutions to the root cause when most remedies lie so easily within our grasp, namely in what we eat and drink. If we choose not to be more scary when discussing today’s plague, how are we ever going to stop it from simply growing and growing, injuring and eventually shortening the lives of millions more people. While dietitians, doctors and other vested interests tackle the symptoms of hyperinsulinemia without acknowledging or even recognizing the cause, and experts feud over the carbohydrate-insulin model of obesity, the plague continues to collect its victims. The historian Suetonius informed us that Emperor Nero watched from a tower while Rome burnt, playing an instrument, giving rise to the expression that he was ‘fiddling while Rome burns’. There is a great danger that while more and more inhabitants of this planet succumb to hyperinsulinemia related illnesses, the mainstream medical community is also in effect, ‘fiddling’, just like Nero did nearly 2,000 years ago. Notes:
At the time of writing, Britain’s NHS has no mention of insulin-resistance or hyperinsulinemia on its website. https://www.nhs.uk/search/ The risks of having hyperinsulinemia include: Higher triglyceride levels, High uric acid, Hardening of the arteries (artherosclerosis), Weight gain, Hypertension, Type-2 diabetes. https://www.diabetes.co.uk/hyperinsulinemia.html This policy brief explains the double burden of malnutrition now facing many countries worldwide – characterized by the coexistence of undernutrition along with overweight, obesity or diet-related noncommunicable diseases (NCDs). https://www.who.int/nutrition/publications/doubleburdenmalnutrition-policybrief/en/ Specific Sources: Shanik, M, et al. 2008: “Insulin Resistance and Hyperinsulinemia. Is hyperinsulinemia the cart or the horse?” Diabetes Care 2008 Feb; 31(Supplement 2): S262-S268. https://doi.org/10.2337/dc08-s264 Crofts, C et al. 2015: Hyperinsulinemia: A unifying theory of chronic disease? https://care.diabetesjournals.org/content/31/Supplement_2/S262 https://www.diabesity.ejournals.ca/index.php/diabesity/article/view/19 Pahdi, T. 2013: Metabolic Syndrome and Skin: Psoriasis and Beyond https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3726879/ Study reveals link between psoriasis and type 2 diabetes (2016) https://www.diabetes.co.uk/news/2016/may/Study-reveals-link-between-psoriasis-and-type-2-diabetes-97737508.html Gyldenløve, M et al. 2015: Patients with psoriasis are insulin resistant https://doi.org/10.1016/j.jaad.2015.01.004 https://www.sciencedirect.com/science/article/abs/pii/S0190962215000079 Ip W, Kirchhof M, G. 2017: Glycemic Control in the Treatment of Psoriasis. Dermatology 2017;233:23-29. doi: 10.1159/000472149 https://www.ncbi.nlm.nih.gov/pubmed/28538228 Other sources: IDF Consensus Worldwide Definition of the Metabolic Syndrome https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome Ultra-processed food - Fresh evidence links popular processed foods with a range of health risks https://www.bmj.com/content/365/bmj.l2289 Doctors of the Black Death - The infamous plague doctors of the Middle Ages were a fearsome sight http://www.doctorsreview.com/history/doctors-black-death/ Pacific islanders pay heavy price for abandoning traditional diet https://www.who.int/bulletin/volumes/88/7/10-010710/en/ Type 2 diabetes, once considered rare in Inuit communities, is now comparable to rates in the general population. https://www.cbc.ca/news/health/inuit-type-2-diabetes-gap-worsens-1.1044126 The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing https://www.cambridge.org/core/services/aop-cambridge-core/content/view/2A9776922A28F8F757BDA32C3266AC2A/S1368980017000234a.pdf/un_decade_of_nutrition_the_nova_food_classification_and_the_trouble_with_ultraprocessing.pdf Dr Unwin’s NICE Endorsed Sugar Equivalence Infographics https://phcuk.org/wp-content/uploads/2019/05/Common-Breakfast-13.05.2019.pdf Harvard researchers studied more than 25,000 American kids — and made a worrisome prediction about what they'll be like by age 35 https://www.businessinsider.com/more-than-half-of-us-kids-will-be-obese-by-35-2017-11?r=US&IR=T Cancer Research UK accused of 'fat shaming' over obesity smoking campaign https://www.telegraph.co.uk/science/2019/07/04/cancer-research-uk-accused-fat-shaming-obesity-smoking-campaign/ Type 2 diabetes drug helps psoriasis, too https://www.psoriasis.org/advance/type-2-diabetes-drug-helps-psoriasis-too Some Definitions: NCD – Non-communicable disease Definition of Plague – “a serious, potentially life-threatening infectious disease that is usually transmitted to humans by the bites of rodent fleas”. https://medical-dictionary.thefreedictionary.com/plague Metabolic syndrome - the medical term for a combination of diabetes, high blood pressure and obesity. https://www.nhs.uk/conditions/metabolic-syndrome/ Hyperinsulinemia - Hyperinsulinemia is most often caused by insulin resistance — a condition in which your body doesn't respond well to the effects of insulin. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/expert-answers/hyperinsulinemia/faq-20058488 Pandemic - A pandemic is an occurrence of a disease that affects many people over a very wide area. https://www.collinsdictionary.com/us/dictionary/english/pandemic Diabesity - Molecular links between Obesity and Diabetes = “Diabesity” https://www.ncbi.nlm.nih.gov/books/NBK279051/
6 Comments
Lizzy Benton
7/14/2019 05:20:16 pm
I read your blog today with great interest, particularly as it revealed what i have been suspecting for a while now, that my husband who two years ago had his first arthritis flare, may have harboured hidden hyperinsulinemia for many years.
Reply
7/15/2019 02:49:03 pm
Thank you Lizzy for your response. My wife recently had a blood test and here in Belgium, we can now request a measure of insulin levels as well as the the more normal fasting blood sugar. She has never had high blood sugars but the insulin level was elevated. That being said, the doctor was more concerned with slightly elevated LDL cholesterol - still a favourite for treatment!
Reply
Lizzy Benton
7/15/2019 04:16:50 pm
Hi Sammy
Reply
Sammy Pepys
1/22/2020 10:09:45 am
Dr Ken Berry has posted his views on nomenclature as follows,
Reply
10/9/2022 10:05:29 pm
Produce company ahead matter off tax. South rock building true. Table note technology quite build great. Throughout all answer skill of generation as.
Reply
Leave a Reply. |
Sammy Pepys"FAT IS OUR FRIEND" ADVOCATES A DIET: Sammy Pepys was the pseudonym used by James Capon when writing this book. He is not a doctor or a nutritionist but has studied nutrition and holds an MPH from Edinburgh University. Over the years, he has become increasingly suspicious of today's conventional wisdom about diet and health. When it comes to what we eat, he has helped many learn to eat more healthily.
Archives
May 2020
CategoriesArchive
|
||||||||||||||||||||||||
| 1_blog_march_2014.docx | |
| File Size: | 546 kb |
| File Type: | docx |
| 2_blog_april_2014.docx | |
| File Size: | 245 kb |
| File Type: | docx |
| 3_blog_may_2014.docx | |
| File Size: | 642 kb |
| File Type: | docx |
| 4_blog_june_2014.docx | |
| File Size: | 426 kb |
| File Type: | docx |

 RSS Feed
RSS Feed